Admittedly, the title is striking. Of course, emotional suffering is a mental problem and has processes in the brain. However, it will be difficult to claim that someone suffering from depression due to thyroid dysfunction has a mental illness. Once the thyroid dysfunction is corrected, the depression also disappears. The reason for the suffering was in the body and was corrected there. This principle applies not only in the case of thyroid dysfunction, but to most mental ailments.
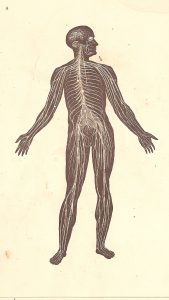
The health insurance system has two offers for people suffering from so-called mental disorders: psychoactive substances for symptom suppression and talk therapy, which is about understanding and also symptom reduction. There is no offer for healing. This is because there is a misconception of the problem. Both approaches believe the core of the problem to be in the brain, medically as neurochemical imbalance and psychotherapeutically as cognitive distortions. Although there is some truth to this phenomenally, the cause lies elsewhere: in the autonomic nervous system (ANS).
Usually the ANS is divided into the sympathetic and parasympathetic nervous system. The sympathetic nervous system is for activation, and the parasympathetic nervous system is for relaxation. Steven Porges’ polyvagal theory makes a further distinction: The parasympathetic nervous system is divided into a ventral branch and a dorsal branch. This dorsal vagus is evolutionarily older and present in all reptiles. Overactivation serves to remain motionless when life is in danger and is responsible for immobilization (stall reflex). The ventral vagus, on the other hand, is present only in mammals. It is responsible for a sense of security, sociability, and social engagement. The branches are, so to speak, two opposite poles of the nervous system with the intervening sympathetic nervous system mobilizing energy for fight and flight (or even for play with simultaneous activation of the ventral vagus). The polyvagal theory is often accused that its biological details are not scientifically proven. However, this circumstance does not take away from the fact that trauma therapy informed by the Polyvagal Theory is able to translate into healing and it offers the best model of the nervous system that we have. To understand our psychodynamics, we don’t need polyvagal theory to be a detailed physical fact, but a foundational outline.
Common mental disorders are usually trauma symptoms. Mental ailments are usually based on a dysregulated nervous system. As a result of trauma, the sympathetic nervous system is chronically activated with a high charge. It permanently holds a fight-or-flight energy that cannot be released by volitional decision. The result is emotional imbalance and lack of stress resistance. At the moment of shock trauma, the dorsal vagus jumps directly into overactivation to ensure survival in the situation. In the case of structural trauma in the sense of developmental trauma, the more the unresolved energy in the sympathetic nervous system charges, the higher the likelihood of overactivation of the dorsal vagus – a desperate attempt by the body to establish balance. In both cases, the nervous system gets stuck in the constellation. The result is dissociation, disproportionate anxiety and depression. The internal body state of the dysregulated constellation of the nervous system is neuroceptively projected onto the external world (i.e., people and situations) over and over again, regardless of how long ago the traumatization occurred and how little danger the external conditions actually pose.
A held charge of strong emotion and a consequent freeze state are the basic state of a traumatized person. Developmental trauma is caused by the parents’ inability to meet the child’s needs for security. It is enough for traumatization if a crying child is left alone or the mother is not accessible for adequate connection due to her own traumatization. Unresolved trauma is unconsciously passed on to the next generation. Anger increasingly builds up in the child, but its expression to the parents is associated with separation and thus with danger to life. As a result, the child dissociates the anger and projects it onto himself. Surpressed anger gets compressed into wrath or hate and probably shows itself in the form of the mental symptom, for example “I hate myself/life” in depression, hearing evil voices in schizophrenia or extreme self-critique in OCD.
Shock trauma is easier to resolve in that only a particular fight-or-flight reflex could not be completed, whereas in developmental trauma the nervous system has successively developed into the dysregulated state. It is important to understand that the nervous system did not do something wrong. It behaved in a way that ensured survival in the best possible way in the particular traumatic situation. Accordingly, it is not that there is something fundamentally wrong with people suffering from mental disorders. On the contrary, they are heroes who have survived highly stressful situations. Only the nervous system has no understanding of time and therefore cannot resolve the dysregulation by itself.
How the brain processes the dysregulation of the ANS depends on genetic disposition as well as on the specific conditions of traumatization. However, the initial situation is always the same. Recurrent depression, forms of anxiety disorders, social disorders, obsessive-compulsive disorders and personality disorders are based on the dysregulation of the ANS. Autism is a special case and is left out here. How often developmental trauma underlies ADD remains debatable, but it can definitely be the basis. Schizophrenia is also a special case. In psychotic states, the brain has become enormously detached from the nervous system and increasingly spins its own story. The trigger for this can be a traumatization, how often this causality exists is open. But one thing is obvious: without traumatization there is no personality disorder, no recurrent depression, obsessive-compulsive and anxiety disorders. Like “I hate myself/life” in depression, hearing evil voices in schizophrenia or extreme self-critique in OCD. Since primary traumatization happens in the first years of life and possibly even prenatally, it usually cannot be remembered. Also, a dependence disorder is often due to a dysregulated ANS, since the nervous system is brought into regulation with the help of the substance.
It is of course useful if people are able to better understand their life situation through classical talk therapy and become aware of cognitive distortions. It is also OK for people to turn to psychoactive substances to improve quality of life and reduce excessive demands. But it must be understood by clinicians, therapists and clients alike that healing does not happen at these levels. It is not possible to resolve deeply ingrained survival strategies via cognition. And any regulation of the ANS produced via psychoactive substances is only temporary.
Healing is possible and it is mainly a somatic process. This is basically good news: healing does not require much thinking or remembering of the past. Instead, one needs innovative connection experiences with people that feel safe and override the trauma pattern, as well as well-dosed reconnection with dissociated feelings without identificatory attachment. Healing is the transference of stuck fight-or-flight energy into flowing life energy and activation of the ventral vagus through human connection. Trauma therapists trained in Somatic Experiencing or the Neuroaffective Relational Model can be of great help in this process. Floating according to Gopal Norbert Klein is another method that can achieve a lot in a short time. Unfortunately, the relevant offers are still very rare and usually have to be paid for by the patient.
So-called mental disorders are therefore not diseases of the psyche, but an expression of a dysregulated nervous system. The sympathetic nervous system is overloaded with fight-or-flight impulses and the dorsal vagus causes freeze and dissociation. The story the brain spins from this is secondary and, accordingly, a symptom. When the nervous system is transferred to regulation, the psyche no longer has a basis for those various disturbance phenomena. How long will it take until the therapeutic mainstream recognizes this and aligns itself accordingly?
Literature:
Dana, D.: The Polyvagal Theory in Therapy: Engaging the Rhythm of Regulation. 2018.
Heller, L.; LaPierre, A.: Healing Developmental Trauma: How Early Trauma Affects Self-Regulation, Self-Image, and the Capacity for Relationship. 2012.
Klein, G. N.: Heilung von Beziehungen I. 2019.
Porges, S.: Pocket guide to the polyvagal theory. 2017